Run Long, Run Healthy: How Much Running is Too Much, Strategies for Curing ‘Overtraining’, and How Sleep Loss Impairs Heat Tolerance
A new study substantiates the old "10% rule" of returning to training.
How Much Running Is Too Much?
Runners (and coaches) have long debated how fast is too fast when increasing training load. The old-school “10% rule” gets tossed around a lot, but most of the science has focused on weekly load increases. Nobody has really put the spotlight on single-session spikes—those days when you go out and suddenly run way farther than usual.
A new study changes that. It gives us some good rules about how to build running mileage when returning from an off-season or injury.
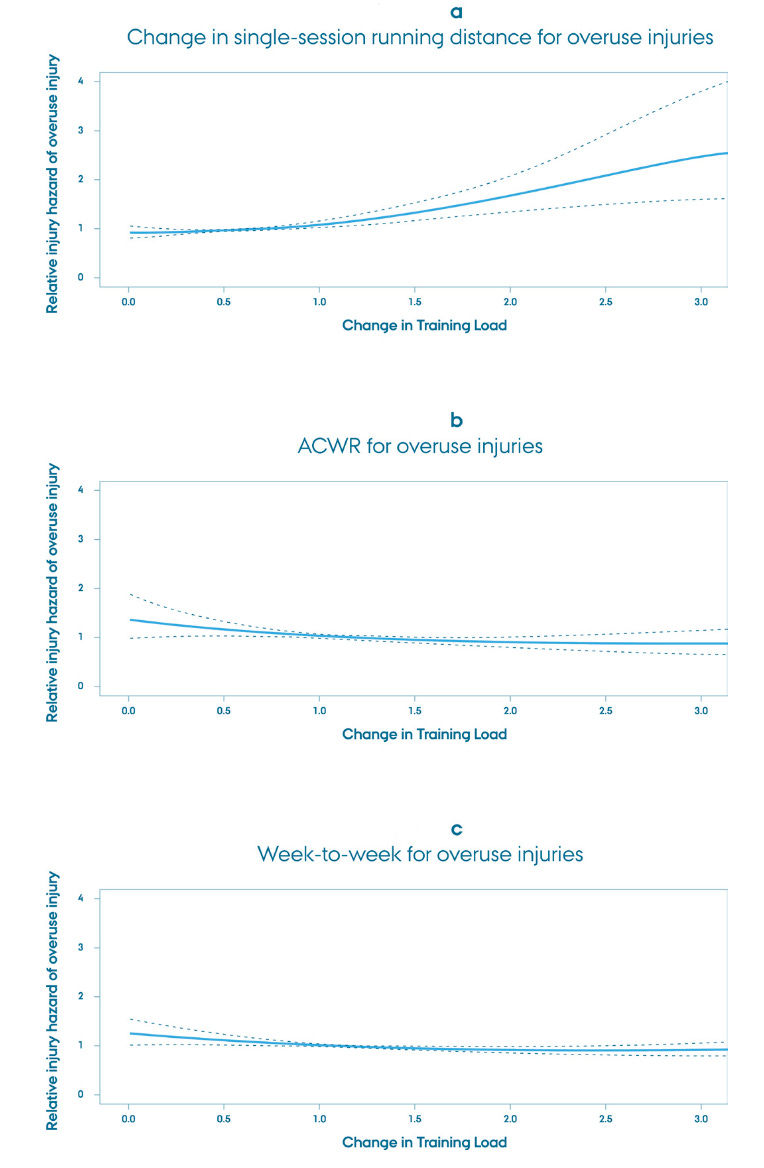
Researchers tracked over 5,200 runners wearing Garmin GPS watches over an 18-month period, gathering data on more than 588,000 running sessions. The primary aim was to figure out whether spikes in training volume—either during a single session or over the course of a week—led to higher injury risk. Importantly, the team differentiated between injuries that developed gradually (classic overuse) and those with traumatic mechanisms (like falls or sprains). They categorized changes in training volume in three ways:
Single-session spike: Comparing the distance of a run to the longest run in the previous 30 days.
Acute to chronic workload ratio (ACWR): A ratio of the most recent week’s mileage to the average of the prior 3 weeks.
Week-to-week ratio: Comparing one week to the week before it.
They then bucketed runners into progression categories: a regression or a 10% or less increase (this served as the reference group), a small spike (>10% to 30% increase), a moderate spike (>30% to 100% increase), and a large spike (>100% increase).
Single-session spikes were strongly predictive of injury, and the risk scaled with the size of the spike. Small spikes in single-session volume were associated with a 64% higher injury risk, moderate spikes were associated with a 52% higher injury risk, and large spikes were associated with a 128% higher injury risk.
On the other hand, weekly changes in mileage weren’t predictive of injury at all. In fact, runners with higher ACWR values (i.e., big weekly jumps) sometimes had a lower injury risk. And week-to-week ratio changes showed no clear association either.
This led the authors to propose the single-session paradigm. Forget week-based calculations. Your injury risk seems to hinge more on how much you increase in one go than on the trend across a week. It’s a classic case of “too much, too soon” crystallized into one run.
What this means for runners
If you’ve been using weekly mileage calculators or relying on the 10% rule to guide your training progression, this study suggests a sharper tool may be to watch for single-session spikes, especially those that exceed your longest run from the past 30 days by more than 10%.
Before you stretch that long run or tag on a few extra miles “because it’s nice out” (we’ve all done it), look back at what your body has actually adapted to recently. Running more is great. But running smarter with thoughtful, patient progression might be your best injury prevention strategy.
The Brutal Reality and Slow Recovery of Overtraining Syndrome
Most runners pride themselves on resilience. Tired legs, sore muscles, early mornings—we wear them like badges. But what happens when your body stops bouncing back altogether?
A detailed case series explores that question through the lens of overtraining syndrome (OTS) faced by three endurance athletes. It’s a reminder that overtraining isn’t just “running too much,” but rather, a multisystem crash involving the endocrine, immune, nervous, gastrointestinal, and musculoskeletal systems. And each case is unique.
The case series followed three endurance athletes, each diagnosed with OTS after months (or years) of declining performance, confusing symptoms, and inconclusive labs. Each case illustrates a different trajectory, but they all share a common theme: recovery was slow, nonlinear, and required an extended, highly individualized return-to-run protocol.
Here’s what that looked like:
Case 1: The pro ultrarunner
This individual (a male) trained 20–25 hours per week and raced 100-milers without breaks between seasons. He experienced symptoms including heart palpitations, hyperventilation, infections, muscle cramps, and depression—all of which were initially misdiagnosed as upper respiratory tract infections and stress.
Return protocol
Phase 1: 4 months of total rest—no running, HR capped at 120 bpm, light cross-country skiing allowed.
Phase 2: Began running a few days per week with HR <140 bpm, with intuitive adjustments based on stress and symptoms.
Phase 3: Gradual return to race training at a higher intensity.
The outcome? This runner returned to competition after 15 months but still avoids all-out race efforts.
Case 2: The recreational ultrarunner
This individual (a male) trained 10–15 hours per week and had moved to altitude to train full-time. His symptoms included heart rate suppression, dizziness, insomnia, “brain fog,” hormonal suppression (low testosterone), and migraines. The initial diagnosis was overtraining syndrome plus hypogonadotropic hypogonadism (a condition where the body doesn’t produce sufficient sex hormones).
Return protocol
Initially tried testosterone therapy, which proved to be ineffective.
Later used HRV-guided training, rest, and gut-targeted naturopathy.
Recovery included long periods of rest and an extremely cautious return to training only when symptoms subsided.
They focused on identifying early red flags like hoarse voice, sleep disruption, and HRV irregularities.
The outcome? They fully recovered and surpassed previous training levels, but at 10–15% lower average intensity.
Case 3: The midlife marathoner
This individual (a female) intensified her training during the pandemic, taking no rest days for several months. Her symptoms included stress fractures, gastrointestinal issues, RED-S, amenorrhea, shortness of breath, and mood swings. She was diagnosed with OTS and RED-S after an extensive clinical workup.
Return protocol
Phase 1: Over 2 years of minimal activity. Began with walking and basic core exercises.
Phase 2: Very light strength training after her body composition normalized.
Phase 3: Reintroduction of hiking, then short jog-walk intervals (e.g., 5-min jog, 2-min walk). Medical management included respiratory therapy, altitude restriction, and correction of acid-base imbalances with medications.
The outcome? After 22 months, she was running up to 45 minutes continuously, slowly resuming structured marathon training, although she still experiences episodic setbacks.
What this means for runners
This study offers several critical lessons. For one, recovery is not linear. All three athletes experienced setbacks, relapses, and false starts. Second, overtraining requires full rest. Each athlete began with complete cessation of cardiovascular exercise, often for months. Third, in the return phase, heart rate and RPE should be the main guides (keeping heart rate below 60% of max and RPE at a ~3–4/10 and running volume should increase before intensity does. Finally, realize that fitness shouldn’t be the only marker of successful progress—mood, sleep quality, hormone levels, gastrointestinal function, and HRV (among other things) should also be tracked.
Let’s be clear: true overtraining syndrome is rare. But if your performance is mysteriously declining, especially alongside systemic symptoms like depression, gut issues, or hormonal disruption, it may not just be stress. And if you're coming back from overtraining, there’s no hack, shortcut, or quick fix. You earn your recovery one low-intensity session at a time.
Sleep Deprivation and Hot Runs Are a Dangerous Combination for Older Athletes
Poor sleep can make a workout feel harder. But for older adults training in the heat, sleep deprivation may do more than sap motivation; it could impair thermoregulation and increase the risk of heat-related illness. That’s the concern raised by a tightly controlled study, which explored how a night without sleep alters the body’s ability to shed heat during exercise.
Researchers had 10 older males (average age 61) complete two trials: once after a normal night of sleep, and once after 24 hours of total sleep deprivation. In both conditions, participants performed three 30-minute bouts of cycling in a hot, dry environment (40°C/104℉, ~13% humidity). Exercise intensity ramped up in each stage: from moderate to intense levels of metabolic heat production.
After sleep deprivation, participants had significantly reduced peak heat loss during the most intense stage of exercise—about 12 W/m² less than when well-rested. That might not sound like much, but it added up to a notable increase in heat storage, about 0.6 kJ/min more than after normal sleep.
Interestingly, evaporative heat loss (the body’s main cooling method via sweat) was almost lower but didn’t reach statistical significance. Dry heat exchange (from radiation and convection) wasn’t meaningfully different.
What this means for runners
If you're in your 50s, 60s, or beyond, sleep matters more than you think, especially in hot weather. This study shows that even one night of total sleep deprivation can impair your body’s ability to offload heat during strenuous workouts. So if you're planning a hard workout in the heat and had a rough night of sleep? It may be smarter to shift the session, lower the intensity, or train in cooler conditions (move that interval session to the treadmill).
How to Use Hill Repeats to Run Faster
Hill repeats are a staple of many successful running training plans. They’re equal parts power and punishment. And if you’ve ever wondered whether the steepness of the hill actually matters for performance gains, a new randomized controlled trial has the answer.





